Physiotherapists are often asked this question. If you’ve ever experienced or currently have a clinically diagnosed disc injury to your lower back you will likely understand why.
There are two usual mechanisms intervertebral discs can become a source of pain.

1. Annular Tear
In the 1950’s it was discovered that discs actually have a nerve supply. Prior to that time, the tiny nerves that supply the outer fibres of the disc (annulus) had never been seen therefore the disc was thought to be insensitive to pain. Other researchers have since determined that there is an overlap of these nerves (sinuvertebral nerves) up to 3 spinal discs above and below the affected disc. Following these discoveries we now believe that the disc can (sometimes) be a source of pain, this pain can be poorly localised and (surprisingly) the disc may be unusual in human musculoskeletal tissue in that the pain may mimic visceral pain (ache) more so than usual orthopaedic pain (like a sprained ankle or torn muscle).
Annular disc injuries may result from progressive change though they can also be caused by trauma. Disc injuries in individuals will often respond favourably to physiotherapy interventions including guided exercises although patience and persistence are key (*please remember this).
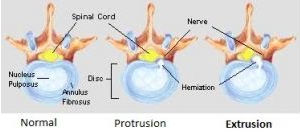
2. Disc extrusion or protrusion
The second mechanism occurs when an extruded or protruded disc contacts spinal nerves or their coverings. In the lower back, this can cause unrelenting and severe pain into the legs as well as sensory changes and muscle weakness in the lower limbs. Amazingly, pressure onto nerves by disc demonstrated on MRI can also be pain-free.
There is a common misconception that if there is material from a disc pressing against nerve tissue that it never heals. This is patently false. Discs can recover if the conditions for healing are created.
The natural process of the human body to clean up extruded material from the disc is called resorption and the pace of which this occurs can vary between individuals. This can be affected by genetics, general health, smoking status & whether your activities or postures (especially repetitive bending and prolonged sitting) continue to create excessive pressure on the injured part of the disc.
It is interesting to also note that MRI findings of improvement will lag behind the improvement of leg symptoms (Ito, 1996) and that the larger the disc injury the more likely it is to resorb (Maigne 1992, Bush 1992, Jensen 1996).
The most hopeful part about this information is that surgery to remove the disc material from the nerve root is no longer considered an early essential treatment measure in most cases.
Surgery should be considered for a disc extrusion or protrusion if there is a change in bowel or bladder function (incontinence or retention) or numbness in the saddle area near the genitals or anus.
Otherwise, surgery is considered elective and is indicated only if:
- Progressive weakness of leg muscles is occurring & numbness is evident in the skin of the leg, and/or
- The pain is not manageable with conservative care (*see note above re patience and persistence).
Conservative care for any disc injury can include physiotherapy interventions, protected weight-bearing exercise, rest from aggravating activities & postures as guided by your physiotherapist and short-term pain-relieving medication or injections into the affected area if required. Examples of protected weight-bearing exercises include hydrotherapy and Clinical Pilates guided by a physiotherapist to be performed with gravity reduced in the vertical plane.
It is very important to have these injuries prescribed on a personal basis as not all will respond to the same set of exercises or activity modifications. One way to explain why is because disc injuries can occur in a 360-degree plane so movements recommended as safe or useful in a particular direction for one person will likely not automatically suit another. This is one reason why Clinical Pilates programs are tailored to the individual.
If this happens to be your situation, you should consider:
- Seeking guidance from a physiotherapist,
- Following through comprehensively with your rehabilitation (this usually changes as recovery progresses),
- Incorporating healthy physical activity into your life
- Avoiding provocative actions such as prolonged sitting, repeated bending or lifting with a flexed lower back (often pain may be delayed so a physiotherapist can guide you to determine the best response for you)
Then you:
- Can be confident that your body will be working to help find the solution.
- Will reduce the rate of recurrent episodes
- Will give your disc the best chance of a full recovery.
And worth noting:
Around 50% of adults of all ages without back pain have disc abnormalities on MRI with up to 30% having protrusions and 1-2% having the more severe extrusion. This likelihood increases with age. If you have lower back pain but no leg symptoms, the occurrence of disc abnormality on MRI may be coincidental and not necessarily linked to your pain (Jensen et al, 1994). If this is you then physiotherapy and appropriate exercise should be your first choice treatment option.
To see one of our physiotherapists call us at 9751 0400 to make an appointment. Our physiotherapist will guide you as to whether manual therapy, exercises, activity modification, Clinical Pilates, or a combination of these (most commonly) is appropriate. Education regarding how to respond effectively to your pain or movement problem is key to your recovery.
